2 Comments
-
Eduardas Vaigauskas
Cancer cells do not “know” in a conscious sense that they need to change their abnormal proteins. Instead, this process happens through natural selection within the tumor as it grows and interacts with the immune system. Several key mechanisms contribute to cancer cells developing resistance to immune system attacks:
• Immunoediting: Over time, cancer cells that are recognized and targeted by the immune system are more likely to be eliminated, while those with mutations that allow them to evade detection survive and proliferate. This process, called immunoediting, leads to the selection of cancer cells with reduced antigenicity, meaning they express fewer or less detectable abnormal proteins.
• Antigen Loss: Some cancer cells can lose or reduce the expression of the abnormal proteins (antigens) that initially triggered the immune response. This can occur through mutations in genes that encode for those proteins, leading to cells that are less visible to T cells.
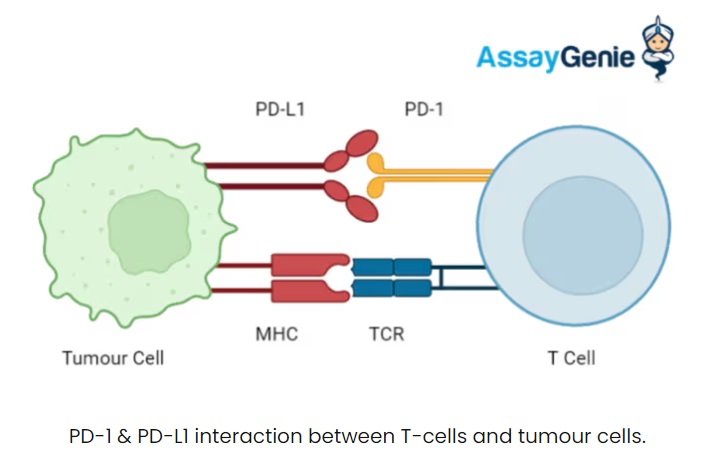
• Downregulation of MHC molecules: Cancer cells can downregulate or alter the expression of major histocompatibility complex (MHC) molecules, which are crucial for presenting abnormal proteins to T cells. Without proper MHC expression, the immune system cannot recognize and attack these cells effectively.
• Expression of Immune Checkpoint Proteins: Tumors often upregulate immune checkpoint proteins like PD-L1, which bind to receptors on T cells (e.g., PD-1) and deactivate them. This allows cancer cells to essentially “turn off” the immune response, preventing T cells from attacking.
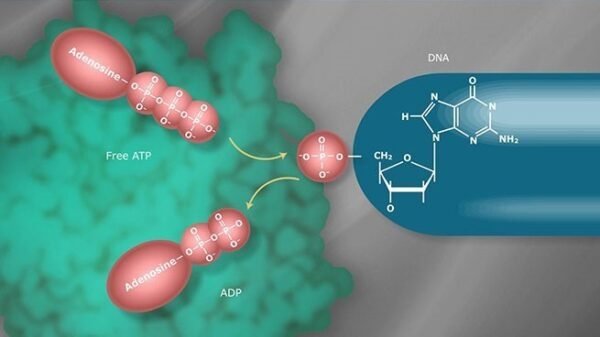
• Mutation of Immune Evasion Genes: Cancer cells can acquire mutations in genes that regulate immune evasion, such as those involved in the immune checkpoint pathway. These mutations may enhance their ability to escape immune surveillance.


Eduardas Vaigauskas
At early stages, cancer cells with high germline epitope burden (those displaying many abnormal proteins or “antigens”) are more likely to attract immune surveillance. The immune system, particularly T cells, recognizes these abnormal proteins as foreign and attempts to eliminate the cancer cells. However, the process is not always perfect. Several factors can prevent the immune system from completely eliminating all cancer cells with high epitope burden:
• Tumor microenvironment: Some areas of the tumor may have a microenvironment that suppresses immune responses, allowing certain cancer cells to evade detection.
• Immunosuppressive factors: Tumors often release molecules (e.g., cytokines like TGF-β, IL-10) that suppress immune activity, reducing the effectiveness of immune cells in clearing all cancer cells.
• Variability in immune system strength: Not all immune systems are equally effective. Factors like the patient’s age, genetic makeup, or pre-existing health conditions can affect how well the immune system responds to early cancer cells.
Thus, while many cells with high germline epitope burden may be eliminated, some may escape immune surveillance, surviving and continuing to grow.